UK Pain Key Messages
There are a large number of messages used for chronic pain by a variety of organisations
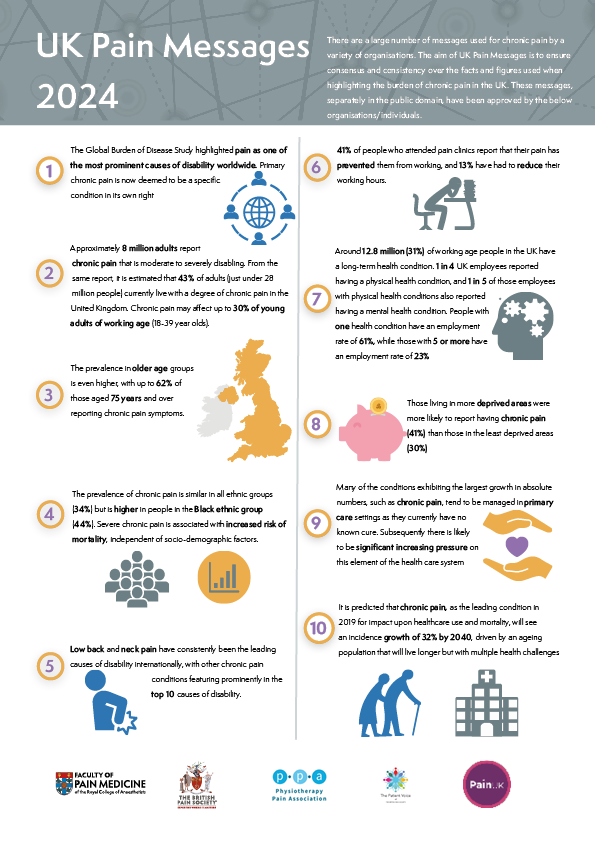
The aim of the UK Pain Messages is to define and gain consensus and consistency over the facts and figures used when highlighting the burden of Chronic Pain in the UK.
These messages, separately in the public domain, have been approved by the following organisations/individuals: the Faculty of Pain Medicine, the British Pain Society, the Physiotherapy Pain Association and importantly patients via Pain UK and the BPS Patient Voice Committee.
Since the last document version in 2017, much has changed in the recommended management of pain with a more conservative approach now given to the use of opioids for chronic pain and the legal reclassification of the gabapentinoids in 2019 as Schedule 3 Controlled Drugs; the intrusion of COVID -19 into all our lives and Long COVID for some; NG 193 guidance on assessment and management of Chronic Primary Pain; the steady shift towards personalised, holistic care and perhaps a need for pragmatic health care given the ever increasing complexity of symptom presentation and significant co-morbidity at scale.
An infographic with these key messages has been developed and is available below to view and download.
It is predicted that chronic pain, as the leading condition in 2019 for impact upon healthcare use and mortality, will see an incidence growth of 32% by 2040, driven by an ageing population that will live longer but with multiple health challenges.
Key Messages
- The Global Burden of Disease Study highlighted pain as one of the most prominent causes of disability worldwide.1 Primary chronic pain is now deemed to be a specific condition in its own right.2
- Approximately 8 million adults report chronic pain that is moderate to severely disabling.3 From the same report, it is estimated that 43% of adults (just under 28 million people) currently live with a degree of chronic pain in the United Kingdom. Chronic pain may affect up to 30% of young adults of working age (18-39 year olds).4
- The prevalence in older age groups is even higher, with up to 62% of those aged 75 years and over reporting chronic pain symptoms.4
- The prevalence of chronic pain is similar in all ethnic groups (34%) but is higher in people in the Black ethnic group (44%)*.5 Severe chronic pain is associated with increased risk of mortality, independent of socio-demographic factors.6
- Low back and neck pain have consistently been the leading causes of disability internationally, with other chronic pain conditions featuring prominently in the top 10 causes of disability.5
- 41% of people who attended pain clinics report that their pain has prevented them from working, and 13% have had to reduce their working hours.7
- Around 12.8 million (31%) of working age people in the UK have a long-term health condition. One in 4 UK employees reported having a physical health condition, and 1 in 5 of those employees with physical health conditions also reported having a mental health condition. People with one health condition have an employment rate of 61%, while those with 5 or more have an employment rate of 23%.8
- Those living in more deprived areas were more likely to report having chronic pain (41%) than those in the least deprived areas (30%).5
- Many of the conditions exhibiting the largest growth in absolute numbers, such as chronic pain, tend to be managed in primary care settings as they currently have no known cure. Subsequently there is likely to be significant increasing pressure on this element of the health care system.9
- It is predicted that chronic pain, as the leading condition in 2019 for impact upon healthcare use and mortality, will see an incidence growth of 32% by 2040, driven by an ageing population that will live longer but with multiple health challenges.9
*Ethnicity indicates a shared cultural identity e.g. African Americans, Black British and now reflects a more nuanced understanding of people’s identities.

The British Pain Society is the oldest and largest multidisciplinary professional organisation in the field of pain within the UK. Our multidisciplinary nature is pivotal in making The British Pain Society a uniquely relevant representative body on all matters relating to pain.

Pain UK envisions a world where everyone enjoys living the best possible quality of life, free from or in control of, the ongoing effects of pain. Our aim is to ensure that the voice of people living in pain is heard and to raise awareness of the burden of pain on individuals and society.

The Physiotherapy Pain Association (PPA) champions physiotherapists working across all specialities in contemporary physiotherapy practice, drawing on biopsychosocial and narrative approaches to support people living with pain.

The Patient Voice Committee was created to act in an advisory capacity to the Council of the BPS, ensuring that the views of patients are represented within the Society and in external discussions about pain. Their mission is “To make a difference to the lives of people living with pain and those of their carers by making the views of patients, based on experience, influential in the design and delivery of the care and support they receive, by working with and for The British Pain Society (BPS)”.
References
- Vos T., Allen C., Arora M. Global, regional and national incidence, prevalence and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016:a systematic analysis for the Global burden of disease Study 2016. Lancet. 2017; 390: 1211-1259. [PMC free article][PubMed][Google Scholar]
- ICD-11 International Classification of Diseases 2023. Available at https://www.who.int/standards/classifications/classification-of-diseases
- Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain 1992;50:133–49. (Comment: The Chronic Pain Grade Scale (CPGS) developed by Von Korff and colleagues is a validated, bidirectional tool that assesses the severity of chronic pain, based on its characteristics and the impact on a person’s activities. The scale uses a severity score based on participants’ subjective assessment of their: current pain; worst and average pain over previous six months; pain related disability and pain interference with social and work related activity. An algorithm divides respondents into: low disability, low intensity chronic pain (Grade I); low disability, high intensity chronic pain (Grade II); high disability, moderately limiting chronic pain (Grade III); and high disability, severely limiting chronic pain (Grade IV).)
- Fayaz A, Croft P, Langford RM, Donaldson LJ, Jones GT. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 2016;6:e010364 doi:10.1136/bmjopen-2015-010364. http://bmjopen.bmj.com/content/6/6/e010364
- Chronic pain in adults 2017. Health Survey for England. Public Health England . Available at https://www.gov.uk/government/ publications/chronic-pain-in-adults-2017
- Torrance N, Elliott AM, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Euro J Pain 2010; 14 (4): 380-83 http://onlinelibrary.wiley.com/doi/10.1016/j.ejpain.2009.07.006/abstract
- National Pain Audit Final Report 2010-2012. Dr Foster Intelligence, British Pain Society, Healthcare Quality Improvement Partnership; 2012. Available at: http://www.nationalpainaudit.org/media/files/NationalPainAudit-2012.pdf
- Health Matters:Health and work (2019). Public Health England. Available at https://www.gov.uk/government/publications/health-matters-health-and-work/health-matters-health-and-work
- Health in 2040: projection patterns of illness in England (2023). The Health Foundation. Available at https://www.health.org.uk/publications/health-in-2040 Version 2.5 (Updated September 2023)
Want to know more?
Visit our Standards and Guidelines
pages for further information.