EPM UK
Recognise - Assess - Treat
Essential Pain Management (EPM) UK is centred around this simple acronym - RAT - which provides a memorable structure and standardises the approach to teaching.
What is Essential Pain Management UK?
"EPM - a simple structure to teach a complex subject"
A survey of pain education (Briggs et al) within undergraduate healthcare studies estimated that ‘the identification, assessment and treatment of pain represent less than 1% of the university-based teaching for healthcare professionals’.
The EPM course was developed by Roger Gouke and Wayne Morriss (ANZCA) to fulfil a training need in less-developed countries. It was subsequently adapted for medical student use by Linda Huggins (Auckland, NZ). Since 2014, we have been using the EPM structure in the UK as a mechanism for training medical students, postgraduate doctors and a variety of allied healthcare professionals in pain management.
Within the RAT structure, all aspects of acute, chronic and complex pain can be taught in a clear and concise way. There is no other such structure available in the widely published literature and therefore, we believe that RAT fills a gap in previous training.
Useful and practical course, good interaction and enjoyable
The role of EPM in UK teaching
- To highlight the gap in existing undergraduate and post-graduate training regarding pain management in general, including focus on complex, longstanding pain and appropriate use of medications.
- To raise awareness that pain is a multifactorial condition, which is often poorly managed, is seen across all specialties and that current graduates are under-equipped to manage this substantial cohort of patients.
- To build upon existing basic medical science teaching in pain medicine and to bridge the gap between this and clinical practice.
- To emphasize the benefit of the recognize, assess, treat (RAT) structure as a mechanism for simplifying the complexity of pain and thereby facilitate understanding of pathophysiology, clinical assessment and appropriate biopsychosocial management.
- To encourage the use of a common framework for pain management across all specialties and professions.
- To promote training, which provides the basis for appropriate prescribing and non-medication management decisions, with the aim of reducing the harm to patients currently caused by excessive medication and protect patients from pharmacological harm in the future.
- To improve training of medical teams, resulting in their enhanced satisfaction for a poorly understood group of patients.
- To motivate medical students, qualified medical staff, patients and other interested parties into taking personal action, with the aim of encouraging local and national training curricula/programmes to fill this curriculum gap.
- To provide evidence of need for training in pain management to stakeholders, including local Medical Schools, Deaneries, Royal Colleges, Medical School Council and other national pre and post-graduate training bodies.
I particularly liked the physiology lecture – very informative and interactive – make all lectures like that
Key features of the RAT structure
| Recognise |
Individual and cultural influences on pain presentations Impact of pain on patients, family, society Benefits of effectively managing pain Review of pain pathophysiology |
| Assess |
Site, severity, cause Classification of pain:
|
| Treat |
Non-pharmacological, including the role of psychology in pain experience Pharmacological:
Placebo effect |
Materials for the complete EPM course are freely available via the links below and provide useful insight into the RAT structure but use of the entire course is not mandatory. The RAT core framework can be used as a standard anchor by anyone teaching pain management and new teaching sessions with specific objectives can be easily built within this context. Any existing pain teaching can be framed within the RAT model with ease.
Teaching EPM online
With current limitations on opportunities for face to face teaching, one of our Regional Leads, Dr Venkat Hariharan, successfully adapted EPM to run a virtual course.
Read about his experience and online programme.
You can also access EPM modules as part of the ePain learning programme.
EPM for medical students
The standard package of materials are of an appropriate level and are ready to use for medical students. However, we encourage adaptation, as desired by those providing the teaching. There may be areas to expand or other areas which are covered elsewhere in the curriculum.
Teaching will be based on the principles of EPM when the core framework is included. There is no requirement to use all available course materials. We would suggest and encourage the use of specific learning objectives for UK medical students, as detailed here. These objectives are all covered within the standard EPM course materials.
To read feedback from students who have taken part in EPM courses click here.
EPM for Foundation doctors
The EPM Advisory Group (EPMAG) have also written pain management specific learning objectives for UK Foundation doctors. It is anticipated that the core framework should be included in Foundation level EPM teaching, and that the standard slide set may be used as a basis for the teaching.
In order to complement and build upon medical student teaching in EPM, we would suggest a brief recap of the overall structure and subsequent particular emphasis on the Foundation level learning objectives. How this is achieved will vary, with some centres preferring a half day course and others delivering teaching in multiple shorter sessions.
EPM for anaesthetic trainees and other groups
Providing there is inclusion of the core framework of EPM and using the standard slide set as a basis if desired, the EPM course can be adapted to suit any learning objectives with any group of participants. Case studies can be provided by the teacher or by the participants in order to demonstrate practical use of the structure and to highlight learning points.
Some examples of more complex EPM-based case studies, which may be useful for e.g. anaesthetic trainees can be found here:
- Acute and Chronic Pain Shingles and Post Herpetic Neuralgia case
- Chronic Pain Headache case
- CRPS case
- Phantom Limb Pain case
- Post-operative Pain and Dementia case
- Rib Fracture case
- Fibromyalgia case study
If you would like more information, please email the Faculty at contact@fpm.ac.uk.
Very useful interactive session. I hadn't heard of the reverse pain ladder before
EPM Advisory Group
Within the Faculty, EPM UK is managed by the EPM Advisory Group, with membership as follows:
- Dr Sailesh Mishra ( Clinical Lead)
- Dr Sibtain Anwar (Deputy Clinical Lead)
- Dr Clare Roques (EPM Global Liaison)
- Dr Hoo Kee Tsang
- Dr Naomi Scott
- Dr Helen Makins
- Dr Karen Gilmore
- Dr Venkat Hariharan
- Dr Jonny Rajan
- Dr Alan Fayaz
- Dr William Rea
- Mr James Goodwin (Associate Director of Faculties)
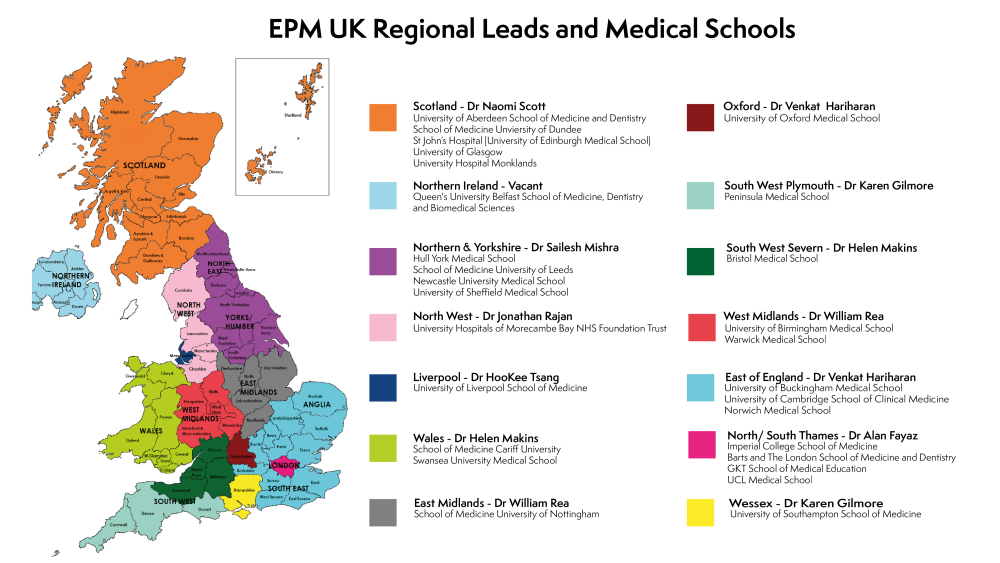
This Advisory Group includes our EPM Regional Leads who work to promote the delivery of EPM throughout the UK. Please see below for regional map, a list of regions and associated Regional Leads.
EPM UK Regional Map
Please see below for a map of the UK with regions, medical schools and regional leads.
| EPM Region | EPM Regional Lead |
|---|---|
| South Western, Severn | Dr Helen Makins |
| South Western (Plymouth) | Dr Karen Gilmore |
| Wessex | Dr Karen Gilmore |
| Wales | Dr Helen Makins |
| Oxford | Dr Venkat Hariharan |
| East of England | Dr Venkat Hariharan |
| East Midlands | Dr William Rea |
| North West | Dr Jonny Rajan |
| North / South Thames | Dr Alan Fayaz |
| Northern Ireland | Vacant |
| Scotland | Dr Naomi Scott |
| Liverpool | Dr Hoo Kee Tsang |
| Northern and Yorkshire | Dr Sailesh Mishra |
| West Midlands | Dr William Rea |
Further Reading for students
EPM Online Resource - this can be used by your students as a follow-on to EPM UK.
Please ensure that University of Auckland, Wayne Morriss, Roger Goucke, and Linda Huggins are all acknowledged each time this resource is circulated or publicised.
Want to know more?
Visit the EPM online resource for more learning materials.