Radiology Corner: Case #2
The second case of the new FPM Radiology Corner investigates Cervical Spine Stenosis and Myelopathy.
Presented by Dr Rhyall Hughes.
Overview
A 58-year-old IT consultant was referred to the pain clinic by his GP with a 2-year history of gradually worsening pain affecting his neck. The GP had trialled Paracetamol and topical Diclofenac gel with little analgesic benefit for the patient. An X-Ray of the cervical spine was requested by the GP in the last month and was reported as showing spondylosis and spondylolisthesis at C5.
On your assessment in the pain clinic, you discover the patient’s pain has increased in intensity and he has started to develop radicular symptoms into both shoulders and upper arms, especially on the left side. He has no red or yellow flags or other significant past medical history of note. He has continued to use Paracetamol and Diclofenac gel but has also started to use Codeine to help while at work. He has made some adaptions to his work environment which have helped reduce his pain while looking at computer screens for long periods of time, although he still has discomfort. He reports significant issues with sleep due to pain.
On examination the patient sits and walks with a slightly stooped posture. He is limited in all planes of movement of his neck due to pain. He has generalised tenderness of the cervical spine with tense trapezius muscles bilaterally. He reports reduced sensation of the C6 dermatome bilaterally but more so on the left. He has normal power and reflexes of his upper limbs.
- What are your differential diagnoses?
- Cervical spondylosis due to
- OA
- Inflammatory arthritis
- Trauma
- Cervical stenosis
- Cervical disc degeneration
- Tumour/mass
- Cervical spondylosis due to
- What investigations would you request at this point?
- Blood test to rule out inflammatory arthropathies
- MRI scan of cervical spine
- What would your management plan be at this point?
- Start anti-neuropathic medication, such as a tricyclic drug
- OT referral to help with work adjustments
- Review in 3-6 months
The patient was started on Amitriptyline 10mg nocte with a plan for his GP to increase up to 30mg nocte as required, to help with sleep and the neuropathic element of his pain. He was referred to the occupation health team, to aid in suitable adjustments for him at work.
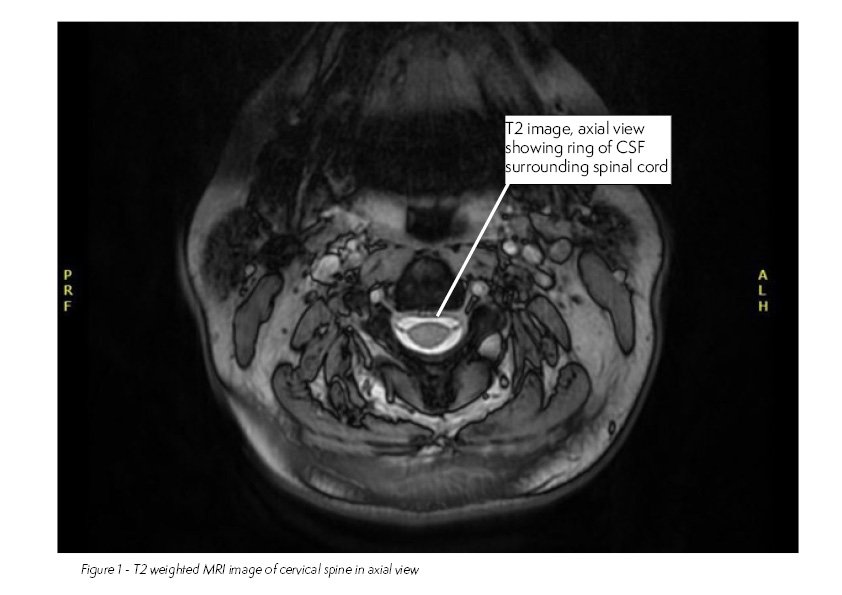
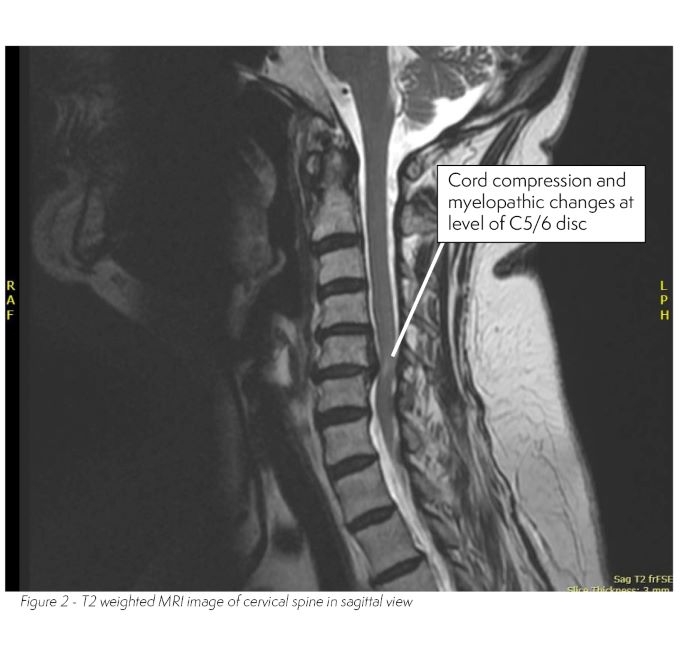
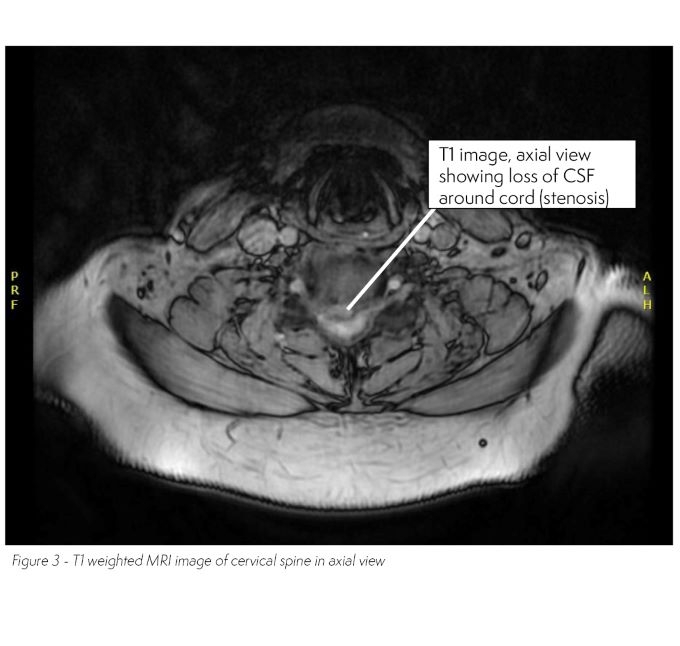
2 months later you review the MRI cervical spine that had been requested.
The bloods you requested show a normal white cell count, CRP and ESR. ANA and ANCA are negative.
- How would these results change your management plan?
- Urgent patient review and assessment
- Urgent referral to neurosurgical team
On reviewing the patient, he describes that over the past few weeks he feels his hands have felt heavy, especially if he has been typing a lot that day. He also reports reduced dexterity and has noticed he is making more typing mistakes than usual. He states that his balance is poor and when he walks barefooted the soles of his feet feel different. He reports some issues with incontinence but was unwilling to elaborate further.
On examination, he has reduced power globally in his upper limbs, with brisk hyper-reflexia in both upper and lower limbs. Plantar reflexes were upgoing on the left hand side.
Diagnosis & Discussion
This patient has developed myelopathic changes of the cervical cord secondary to cervical spine stenosis.
Cervical stenosis is a relatively common condition and has been found to affect 4.9% of the adult population, with increasing incidence with age. Patients’ symptoms tend to slowly deteriorate but rapid deterioration can also occur, though many patients will be asymptomatic. Cervical stenosis can lead to radicular symptoms due to nerve root compression and myelopathy due to spinal cord compression. MRI is the gold standard investigation. Evidence of rapidly progressive neurological deficit warrants urgent neurosurgical review.
Suggested Reading
- Benjamin M Davies, Oliver D Mowforth, Emma K Smith, Mark RN Kotter
Degenerative cervical myelopathy
BMJ 2018; 360 doi: https://doi.org/10.1136/bmj.k186
(Published 22 February 2018) - Lindsay Tetreault, Sukhvinder Kalsi-Ryan, Michael G. Fehlings
Degenerative Cervical Myelopathy: A Practical Approach to Diagnosis
Global Spine Journal (open access) Volume 12, Issue 8, 2022
https://journals.sagepub.com/doi/10.1177/21925682211072847 - Allan R. Martin, Lindsay Tetreault, Shekar N Kurp
Imaging and Electrophysiology for Degenerative Cervical Myelopathy [AO Spine RECODE-DCM Research Priority Number 9]
Global Spine Journal Volume 12, Issue 1_suppl
https://journals.sagepub.com/doi/10.1177/21925682211057484?icid=int.sj-full-text.similar-articles.1
